Sorry, nothing in cart.
Sleep apnea and diabetes are two common ailments in the human body, and they tend to accompany each other at times. Sleep apnea is a situation where a person has their breath interrupted time and again, resulting in disturbed sleep and a shortage of oxygen in the body.
Diabetes, particularly type 2, has something to do with the regulation of insulin in a human’s bloodstream. Both these ailments have seen a rise in their patient population across the globe, owing to a higher rate of people being overweight.
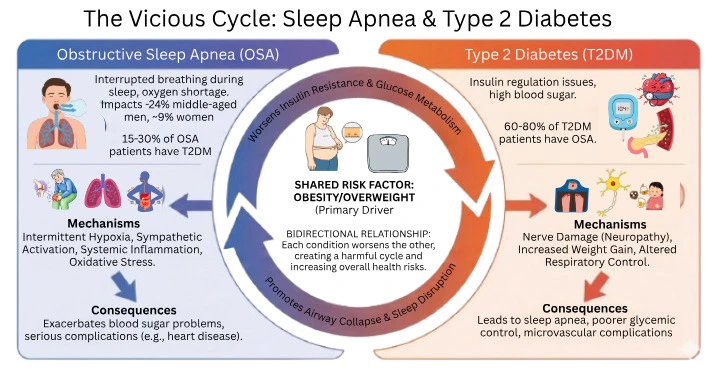
Numerous studies in the field of healthcare reveal the relationship between Obstructive Sleep Apnea (OSA) and Type 2 Diabetes (T2DM).
It was known to impact approximately 24% of middle-aged males and 9% of females. Moreover, 60-80% of patients with Type 2 Diabetes had been known to have Obstructive Sleep Apnea, while 15-30% of patients diagnosed with Obstructive Sleep Apnea were observed to have Type 2 Diabetes.
This is important to grasp because if OSA is not treated, it can lead to the exacerbation of blood sugar problems and even serious complications such as heart disease.
Similarly, if diabetes is not effectively managed, it can lead to problems with sleep apnea as a result of nerve damage and increased weight gain.
What Is Sleep Apnea?
Apnea is a condition of sleep where breathing is temporarily paused from time to time.
Such a time without breathing can last for only a few seconds or can be longer than one minute, and repetition may be very high even throughout one hour of sleep. As a result, the level of oxygen within the lungs is lowered, and the sleep cycle is disrupted.
The main form of SDB is Obstructive Sleep Apnea, by which the relaxation of the throat muscle causes the obstruction of the airway.
Consequently, the person finds breathing laborious and requires the temporary stimulation of the brain, which awakens the person and reopens the airway.
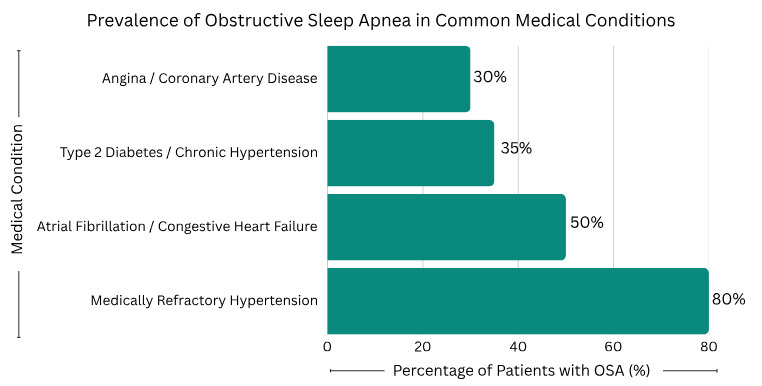
OSA is associated with a number of diseases. The facts state that obstructive sleep apnea can be found to exist within 30% of patients diagnosed with angina or coronary artery disease, 35% of those diagnosed with Type 2 diabetes or chronic hypertension, 50% of those diagnosed with atrial fibrillation or congestive heart failure, and 80% of patients diagnosed with medically refractory hypertension (ResearchGate, 2018). Statistics demonstrate how valuable OSA can be to both cardiovascular and metabolic issues.
Episodes of interrupted breathing provoke the secretion of stress hormones, including cortisol and adrenaline. Regularly, this builds up to higher blood pressure, insulin resistance, and being overweight, which are contributing factors to Type 2 diabetes.
The Connection Between Sleep Apnea and Diabetes
Sleep and blood sugar are closely linked. When sleep is deep and restful, the body balances hormones that control sugar and stress.
But when sleep keeps getting disturbed, the body releases stress hormones that raise blood sugar and make insulin less effective (ScienceDirect, 2017).
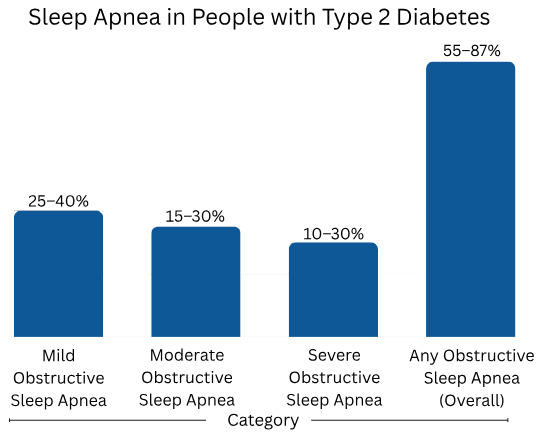
Several studies reveal the correlation between sleep apnea and type 2 diabetes. The data from several countries in the image show that the overall rate of obstructive sleep apnea (OSA) in people with diabetes ranges between about 55% and 87%.
In other words, that’s over 50% of people with type 2 diabetes who also have sleep apnea. Some studies show mild OSA in about 25-40%, moderate OSA in around 15-30%, and severe OSA in 10-30% of people tested.
These numbers show that sleep apnea is not rare – it is very common in diabetes and can vary in how serious it is.
Overview of how sleep and metabolism are linked
People with sleep apnea have their breathing stop a lot at night. Each time it happens, oxygen levels drop, and the brain wakes the body slightly to start breathing again. These repeated drops in oxygen trigger stress hormones that keep blood sugar high. Over time, this constant stress can damage the body’s ability to use insulin properly and can lead to insulin resistance (ScienceDirect, 2017).
Why do these conditions often occur together?
Sleep apnea and type 2 diabetes have a lot of the same risk factors.
Being overweight, older age, and lack of physical activity increase the risk for both. But even without obesity, OSA can affect how the body handles sugar.
The lack of oxygen and poor sleep quality cause the body to store more fat and use insulin less efficiently.
The Bidirectional Relationship
The connection between sleep apnea and diabetes works both ways. Sleep apnea can make diabetes worse, and diabetes can also make sleep apnea more serious (ScienceDirect, 2017).
How sleep apnea worsens diabetes
When a person stops breathing while sleeping, there is a lack of oxygen in the blood.
The body receives a signal to release stress hormones, such as cortisol, in response to low oxygen in the blood. Stress hormones increase blood sugar and make it insulin-resistant.
People with untreated OSA often wake up tired, and their fasting glucose and HbA1c levels tend to be higher than normal.
How diabetes aggravates sleep apnea
Diabetes can also make sleep apnea worse. High blood sugar damages nerves over time, a condition called diabetic neuropathy.
When the nerves that control breathing and airway muscles are affected, the airway can collapse more easily during sleep.
Diabetes also causes inflammation and fluid buildup, which makes breathing harder and narrows the airways.
Can Sleep Apnea Cause Diabetes?
Research shows that sleep apnea may raise the risk of getting type 2 diabetes over time.
This can happen even in people who did not have diabetes before. This puts the body under stress and can affect how it handles sugar.
One study looked at 330 adults with type 2 diabetes and checked for sleep apnea using a sleep test. It found that sleep apnea was very common in this group. Depending on how severe it was, the rate ranged from about 29% to 48%.
The study also reported an overall sleep apnea rate of 36%, with 49% in men and 21% in women (ScienceDirect, 2020).
This shows that sleep apnea is often present in people with diabetes, and it may also play a role in making blood sugar control harder.
Sleep apnea may increase diabetes risk because of what happens during oxygen loss. When oxygen goes down, the brain and body react as if danger is around the corner.
The body goes on to produce stress hormones like cortisol and adrenaline. These hormones raise blood sugar so the body has quick energy.
Difference between direct cause and long-term risk
Sleep apnea does not usually “cause” diabetes in a single day. It works more slowly. The risk builds up when sleep apnea is present for months or years.
Long-term OSA can lead to repeated inflammation, higher stress hormone levels, and frequent sugar spikes during the night. Even mild sleep apnea, if untreated, can slowly push the body toward poor glucose tolerance and insulin resistance.
Role of untreated sleep apnea
It can also raise diabetes risk by keeping blood sugar high and damaging insulin action. Each oxygen drop signals the liver to release more glucose.
At the same time, the pancreas has to work harder to let insulin out. Over time, this constant pressure can make blood sugar control worse and may increase the chance of developing type 2 diabetes.
Because of this, screening is important, especially for people who snore loudly, feel tired in the day, have obesity, high blood pressure, or poor blood sugar control. Finding and treating sleep apnea early may help reduce long-term diabetes risk.
Why Is Sleep Apnea More Common in Type 2 Diabetes?
One major risk is obesity, which is also a major risk factor among OSA patients.There is also the issue of inflammation and insulin resistance.
Factors related to inflammation, including TNF-α and IL-6, can influence the upper airway and glucose.
Another condition, diabetic neuropathy, could potentially impair nerves controlling upper airway muscle contraction to keep the upper airway passage open during sleep.
Physiological Mechanisms Linking OSA to Glucose Intolerance
Oxygen Deprivation and Insulin Resistance
Every time there is an apnea event, it leads to reduced oxygen levels (hypoxia), causing the body to secrete stress hormones, such as cortisol.
Cortisol is known to affect insulin receptors, leading to reduced glucose uptake by tissues and thereby increasing blood sugar levels and precipitating insulin resistance.
Poor Sleep Quality and Glucose Metabolism
Frequent arousals from sleep interfere with the stage of sleep where important metabolic work takes place.
Disrupted sleep leads to increased cortisol release at night and decreased insulin sensitivity.
This implies that even if the individual’s food is in order, the body’s ability to deal with sugar is not ideal, and this increases their levels of fasting glucose and HbA1c.
Does Sleep Apnea Affect Blood Sugar Levels?
OSA affects blood sugar by causing spikes during the night and higher fasting levels in the morning.
Individuals suffering from OSA frequently present with raised HbA1c levels, which is a marker of suboptimal glucose control over time. Studies show that effective sleep apnea treatment can reduce HbA1c by 0.3–0.5% on average (Healthline, 2024).
Nighttime oxygen drops also trigger glucose fluctuations. This “rollercoaster effect” puts extra stress on the heart and blood vessels, making it harder to manage diabetes even with medications like Metsmall SR 500 Mg (Metformin), glimepiride, or insulin.
Recognizing the Symptoms
Common Warning Signs of Sleep Apnea
Diabetes Symptoms That May Indicate Sleep Issues
These overlapping symptoms often mean both conditions need evaluation together.
How can diabetics know They Have Obstructive Sleep Apnea?
Screening tools tend to be as the STOP-BANG questionnaire or Epworth Sleepiness Scale help identify high-risk individuals.
A sleep study, or polysomnography, can confirm the diagnosis by measuring breathing, oxygen, and heart rate during sleep.
Portable home sleep tests are now available, allowing easier diagnosis for diabetic patients who experience fatigue or snoring. Early detection can prevent complications before blood sugar control worsens.
How Is Sleep Apnea Treated?
CPAP Machine
Pressure is the most common and the most effective method of treatment. The method entails the delivery of a mild air pressure that helps to keep the airway open during sleep. Long-term CPAP use enhances sleep quality and has been reported to reduce fasting glucose and HbA1c in diabetic patients.
Oral Appliances
In essence, oral appliances work by repositioning the jaw or the tongue, thus preventing airway obstruction. They are a solution for those with mild to moderate OSA or for patients who cannot use CPAP.
Surgery
When the condition is extremely severe, surgical intervention might be an option where the excess tissue is removed or the structural problems in the airway are corrected.
What Are the Effects of Sleep Apnea Treatment on Diabetes?
Treating obstructive sleep apnea (OSA) can help people better manage their diabetes. When breathing becomes steady at night, the body gets more oxygen, and sleep improves. This can lower stress in the body. With less stress, the body may use insulin in a better way, and blood sugar may become more stable.
CPAP (a sleep apnea mask machine) is the most common treatment. CPAP keeps the airway open so breathing does not stop during sleep.
Many studies show that people who use CPAP regularly can have better blood sugar control. Some people also see lower blood pressure. But results are not the same for everyone.
A big reason is how often and how long CPAP is used each night. If someone uses it only for a short time, the benefit may be small (ScienceDirect, 2017).
Sleep apnea treatment does not replace diabetes treatment. People still need to follow their diabetes care plan. But better sleep can support better daily control.
It may also help the body respond better to diabetes medicines like metformin, Glypride 1 Mg (Glimepiride), Glizid 40 Mg (Gliclazide), and Januvia 50 Mg (Sitagliptin).
Can Treating Sleep Apnea Cure Type 2 Diabetes?
No. Treating sleep apnea does not cure type 2 diabetes. Type 2 diabetes is a long-term condition. It depends on many things, like weight, diet, activity, genes, and how the body uses insulin.
But treating OSA can still help a lot. When sleep apnea is treated, oxygen levels stay more stable, and sleep becomes less broken.
This can lower stress hormones that raise blood sugar. It can also reduce heart risks that are common in both sleep apnea and diabetes.
So, OSA treatment should be seen as support, not a cure (ScienceDirect, 2017).
How to Manage Diabetes with Sleep Apnea
Managing both conditions together works best. The goal is to improve sleep, keep blood sugar steady, and lower the risk of heart disease.
Lifestyle Changes
Small daily habits can help both sleep apnea and diabetes:
Managing Blood Sugar to Improve Sleep
Blood sugar changes at night can disturb sleep. Keeping glucose steady can help you sleep better.
Using Sleep Trackers to Monitor Sleep Quality
Modern sleep trackers can measure breathing rate, oxygen levels, and sleep stages.
They help people with diabetes and OSA monitor their progress. However, these devices cannot replace clinical diagnosis and should be used only as supportive tools.
The Importance of Early Diagnosis and Treatment
Untreated OSA elevates the risk of myocardial infarction, cerebrovascular accidents, and deteriorated glycemic control. Besides, detecting and managing sleep apnea at an early stage averts the development of complications and improves quality of life.
Endocrinologists and sleep specialists working in concert provide the most effective outcomes over time.
Takeaway
Sleep apnea and diabetes share a deep, two-way connection. Poor sleep and low oxygen levels raise blood sugar and insulin resistance, while diabetes worsens breathing problems.
Screening, early treatment, and consistent lifestyle management can break this cycle. For patients and doctors alike, understanding this link is key to better metabolic and cardiovascular health.
